Introduction
Accidental upcoding in medical billing can cause significant financial and legal issues. It might lead to legal issues, fines, and loss of trust with patients and insurers.
Upcoding occurs when providers bill services at a higher rate than they actually delivered. Often, this is unintentional but still comes with serious consequences. To avoid accidental upcoding, healthcare providers and billing teams should follow simple practices and stay updated on coding rules.
Below are easy steps to help prevent errors and keep your billing accurate.
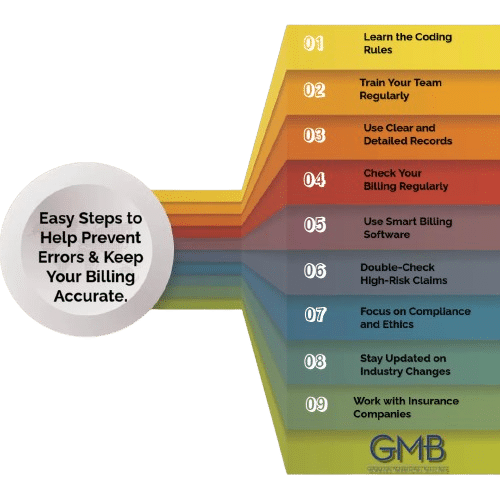
1. Learn the Coding Rules
Accurate coding is key to proper billing. Every billing code has specific rules, and your team needs to know them well. Experts often update CPT, ICD-10, and HCPCS codes. These updates may introduce new rules or change how people use codes.
Key Tip: Certifications from trusted groups like AAPC or AHIMA can help your team stay informed. These certifications teach the latest coding rules and best practices.
2. Train Your Team Regularly
Billing and coding rules often change. If your team doesn’t stay updated, they might make mistakes like upcoding. Training sessions are a great way to refresh their knowledge and keep them informed.
Key Tip: Offer regular training and access to webinars or guides. This keeps your team updated on new rules and coding standards.
3. Use Clear and Detailed Records
Incomplete records are a common reason for upcoding. You must clearly document every service, procedure, or treatment. This helps coders pick the right codes and avoid mistakes.
Key Tip: Use templates for documentation. Templates guide healthcare providers to include all the details needed for correct coding.
4. Check Your Billing Regularly
Audits are a good way to find and fix mistakes. Regular checks can help you spot patterns of accidental upcoding or other issues. Audits also show areas where your team might need more training.
Key Tip: Plan monthly or quarterly audits. Focus on claims that involve higher costs or more complex services.
5. Use Smart Billing Software
Good billing software reduces human errors. Many systems have tools that flag mistakes, like mismatched entries or duplicate codes.
Key Tip: Choose software with built-in compliance checks. Search for systems that alert you to potential coding issues before you submit claims.
6. Double-Check High-Risk Claims
Some claims, like surgeries or long treatments, are more likely to have mistakes. Ask a senior billing team member to review these claims before sending them.
Key Tip: Set up a second review process for high-risk claims. This can catch errors that someone might have missed earlier.
7. Focus on Compliance and Ethics
Compliance means following all the rules, and ethics means doing what’s right. Both should be priorities for your billing team. Teach your staff why accurate billing is important and how upcoding can harm your practice.
Key Tip: Hold team meetings to discuss compliance and billing ethics. Show your staff how accuracy builds trust with patients and insurers.
8. Stay Updated on Industry Changes
Rules for medical billing change often. Groups like CMS (Centers for Medicare & Medicaid Services) release updates that your team needs to know.
Key Tip: Sign up for newsletters from CMS, AAPC, or AHIMA. Share important updates with your team to keep everyone informed.
9. Work with Insurance Companies
Sometimes, billing rules can be unclear. Talking to insurance providers can help you understand their specific requirements.
Key Tip: Build relationships with insurance companies. This makes it easier to solve problems or ask questions when needed.
Conclusion
Accidental upcoding can hurt your practice, but it’s easy to avoid. Train your team, keep your records clear, and check your claims regularly. Use smart billing tools and review high-risk claims carefully.